Drug discovery for new therapies
Bioreactor research processes and cryotechnologies improve active ingredient tests using human cell cultures
Many new drug candidates end up failing because they cause serious side effects in clinical trials even though lab tests involving cell cultures have been successful. This is a common occurrence if the cells used come from animal tissue, for example. Specially prepared cell cultures made from human tissue known as human induced pluripotent stem (hiPS) cells enable greater reliability in testing, thereby also increasing the chances that a drug will be approved. Fraunhofer researchers have developed innovative solutions for optimized production of cells in bioreactors and unique cryotechnologies. This is paving the way for efficient real-world use of these cell cultures in toxicity testing.and drug discovery.

Researchers are faced with a dilemma if participants experience serious side effects during clinical trials to test new active ingredients. Often, this means development of a promising drug candidate will be halted, so the drug never reaches the market. One of the root causes is that drug candidates are typically tested using in vitro cell culture models based on animal cells or on animals first. In either case, there are limits to how well the test results translate to human subjects. That means there is a risk that trial participants will suddenly experience intolerable side effects.
Medical researchers have high hopes for what are known as human induced pluripotent stem (hiPS) cells. These cells originate from human tissue, so they are a much more accurate basis for determining how substances will work in human subjects than conventional tests. The cells are taken from human skin tissue or a blood sample and then undergo a special reprogramming procedure in the lab. After that, they are no longer programmed for a single type of tissue, which is why they are called “pluripotent.” For drug testing purposes, the hiPS cells can then be re-differentiated into almost any kind of cell found in the human body. This significantly lowers the risk of undesirable side effects occurring in subsequent human clinical trials.
Bioreactors for scaled-up cell production
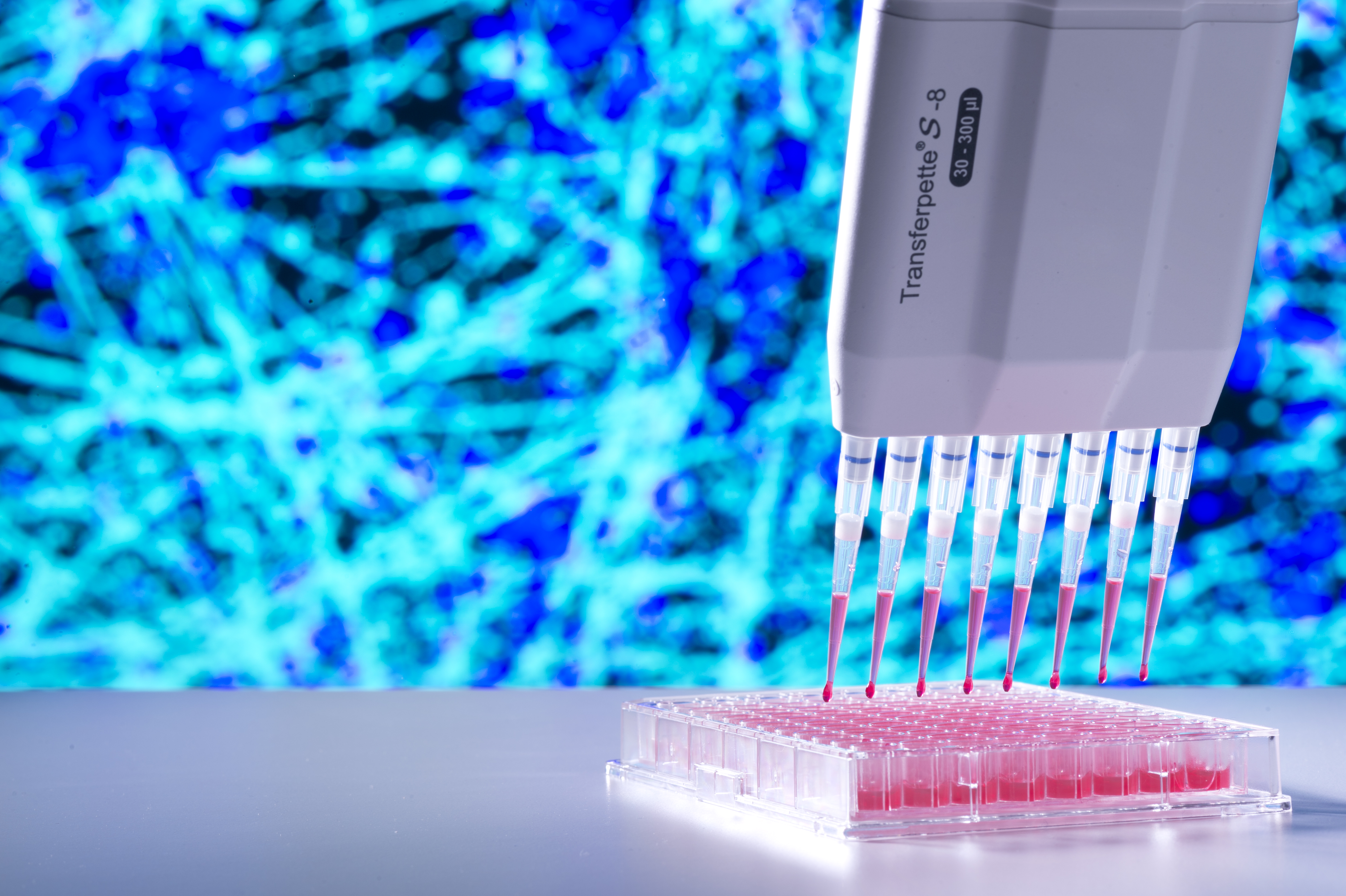
The cells needed for the tests are produced in bioreactors. A team of researchers headed by Dr. Julia Neubauer, head of the Cryo & Stem Cell Technologies department at the Fraunhofer Institute for Biomedical Engineering IBMT, has now made a significant advance in multiplying and differentiating hiPS cells in a bioreactor. “It is now possible for the first time to scale up the process so large quantities of functional cells are created in a short time,” Neubauer says.
The challenge for the Fraunhofer scientists participating in the R2U-Tox-Assay joint project was to find out how best to replicate the environmental conditions naturally occurring in the human body in a bioreactor so the cells multiply quickly without any loss of functionality. “We developed and produced our own elastic hydrogel to act as a substrate specifically for the bioreactor. The cells are right at home there, so they can proliferate effectively. The chosen parameters allow us to produce quantities that are relevant for medical testing of up to several billion cells,” Neubauer explains.
The cell models produced in this way — which can be differentiated into tissues such as heart muscle, skin, or neurons — can then be used in assays for testing drug candidates and determining their toxicity. Another advantage is that the hiPS cells are human cells that still contain the donor’s genome information, which makes it possible to develop appropriate tests of new active ingredients to treat diseases and disorders with a genetic component as well.
Cryotank flash freezing
However, there is another issue for both drug researchers and university medical centers: storage and availability of cell cultures. The Fraunhofer researchers put their decades of expertise in cryopreservation of cells to work on this question.
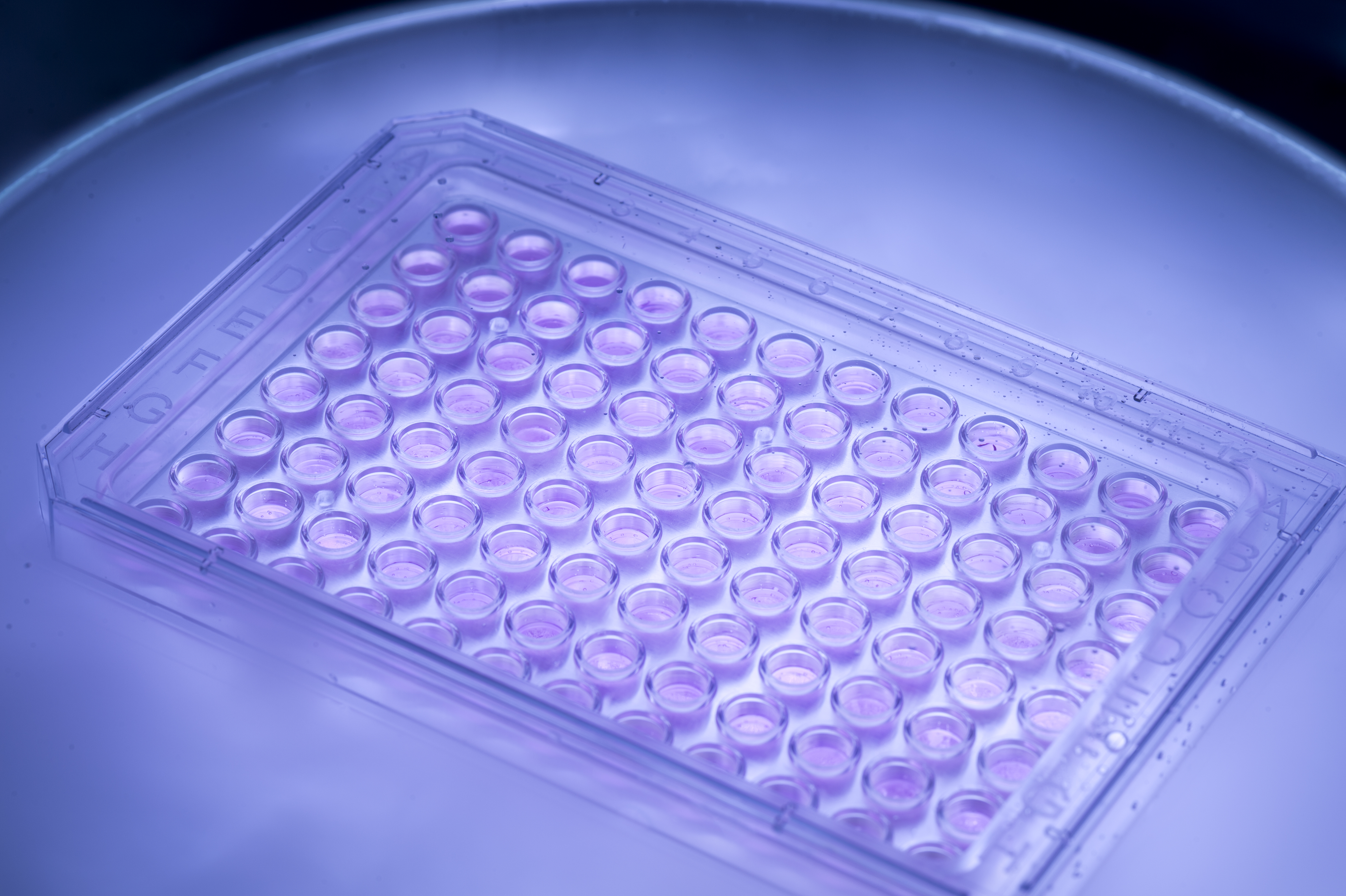
Fraunhofer IBMT has developed cryopreservation methods found nowhere else in the world. Liquid nitrogen is used to cool the cell models grown in the bioreactor from about plus 23 degrees Celsius down to minus 196 degrees within two seconds. The Fraunhofer researchers have also developed a special cell culture plate that can be used to first culture the cells and then freeze them. Combined with the rapid freezing process, special freezing media impair the formation of ice crystals in the cell tissue, which would damage the material and leave it mushy. “If you’ve ever frozen strawberries at home, you’ll be familiar with this undesired effect,” Neubauer says with a smile.
She and her team developed a detailed cryopreservation protocol describing the correct procedure. The protocol sets out parameters, such as cooling speed and the times the freezing media need to take effect, for the specific types of cells to be preserved. These methods ensure that the sensitive human cell cultures will retain their full functionality after they are removed from cryostorage and then thawed. The standardized cell culture plates make it possible to store and transport the cell cultures almost without limitation for the high-throughput screenings used in pharmaceutical research. Hospitals and pharmaceutical labs can keep cell cultures in stock so they always have the right cells available for toxicity and drug testing.
Improved candiate tests for new drugs
The refined bioreactor and cryostorage concepts clear the path forward for efficient real-world use of hiPS cells in medical research. Traditional in vitro tests involving animal cells and ethically problematic animal testing are both replaced by significantly more accurate testing systems. “On the whole, the accomplishments of R2U-Tox-Assay enable more efficient, safe development of drug candidates to treat a range of diseases, including heart and eye diseases and even neurological disorders such as dementia,” Neubauer says.
Fraunhofer IBMT’s partners in the recently concluded joint project were Janssen Pharmaceutica N.V. and the Institute for Bioengineering of Catalonia. The project received funding as an innovation project under the EU’s major EIT Health initiative.